When is Peak Flu Season?
Influenza (flu) season in the United States occurs in the fall and winter. It specifically starts in October and can continue until as late as April. The impact of people infected with the flu varies every year and is also dependent on the number of people who receive the vaccine.
Texas, Oklahoma, and Connecticut have the highest number of influenza cases, based on the activity over the past six years during February (the most recorded cases). The score is then weighted to determine high activity over moderate low. Another factor is the average cost of doctor visits in the state and access to flu care.
When Does Flu Season Peak?
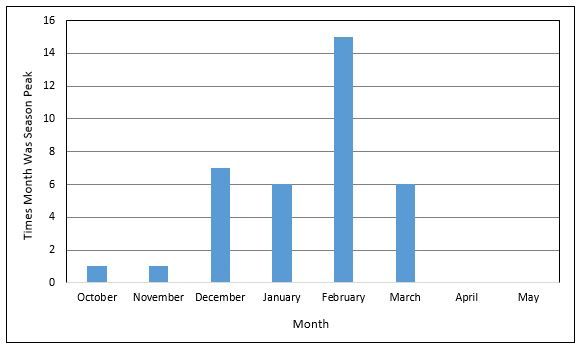
A peak is when the highest amount during a specific amount of time; in terms of the flu season, the peak is reached when the highest amount of cases occurs during the season. Based on the past flu seasons, the peak of flu season for many states is during the first weeks of February.
Below is a graph made by the CDC depicting the monthly distribution of flu seasonal peaks. The graph shows that the seasonal peak is usually in February, sometimes in December, January, or March, and rarely in October, November, April, or May.

Get affordable doctor copay without paying insurance premiums
Join 39,000 people and get Mira, the best alternative to traditional insurance. Enroll and use immediately. Plans start at only $45/mo.
Khang T. Vuong received his Master of Healthcare Administration from the Milken Institute School of Public Health at the George Washington University. He was named Forbes Healthcare 2021 30 under 30. Vuong spoke at Stanford Medicine X, HIMSS conference, and served as a Fellow at the Bon Secours Health System.
